

Hemodialysis
Hemodialysis is a term that means "cleaning the blood." Although there are a few other reasons to perform hemodialysis, such as special kinds of poisoning, it is usually performed in patients who have some type of kidney disease that prevents them from clearing all of the protein byproducts of normal metabolism from their blood. For some patients it may only be required for a short period of time; for most, however, it is a lifelong commitment, at least until a kidney transplant is available.
The process of hemodialysis involves circulating a patient's blood through a machine called a dialyzer. It is a large canister made up of two spaces separated by a thin membrane and contains many small fibers that the blood is passed repeatedly over.
Cleansing fluid is pumped around these fibers to allow the wastes and extra fluids to pass from the patient's blood into the solution, which carries them away. The cleaned blood is returned to the patient's bloodstream. Removing the harmful wastes and extra salt and fluids helps control blood pressure and keep the proper balance of chemicals like potassium and sodium in the body.
How are you attached to a dialysis machine?
There are a few different ways for a patient to be attached to a dialysis machine. The first step before starting hemodialysis is to prepare a site on the body from which the blood is removed and returned. This is called the vascular access site. The vascular access site is usually prepared a few weeks or months before dialysis begins, although with some of the new synthetic grafts, dialysis can begin almost right away.

Internal Fistula
One method of providing permanent access to the bloodstream for hemodialysis is by creating an internal fistula in the arm. A fistula is a bridge or connection between an artery and a vein, usually created by a surgeon. Needles can be inserted in the enlarged vein to connect to the dialysis machine.
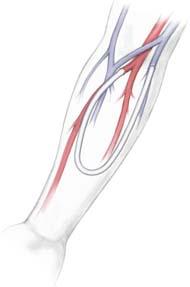
Internal Graft
Another method is to insert an internal graft. This is when an artery is surgically connected to a vein with a short piece of special tubing placed under the skin. Needles can be inserted in this graft.
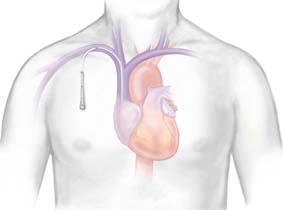
Central Venous Catheter
In some cases if quick access is needed or when the veins in the arms are too small, a central venous catheter is used. This is a soft tube that is surgically inserted into a large vein in the neck or near the collarbone. This method is usually temporary until a permanent access site is ready.
Does hemodialysis hurt?
The most unpleasant part of hemodialysis is the actual insertion of the needles. But over time, it becomes more tolerable and an anesthetic cream or spray can be applied to the skin to help with the discomfort. For patients with a synthetic graft, this discomfort is minimal.
How are the needles inserted?
There are different methods that can be used for needle placement.
- Ladder technique: A "ladder" strategy is when the placement of the needle "climbs up" the entire length of the vascular access area, using a different location each session so that any one location is not weakened by too many needle sticks.
- Buttonhole technique: An alternative approach is the "buttonhole" strategy in which a limited number of sites are used but the needle is inserted precisely into the same hole made by the previous needle stick.
How is the dialysis procedure performed?
The common practice for dialysis is to use two needles; one carries blood to the dialysis machine and the other one to return purified blood to the body. Different types of needles are used including specialized needles designed with two openings for two-way flow of blood. Needles for high-efficiency dialysis are larger than those used with regular dialyzers.
How long does dialysis take?
Hemodialysis treatment normally takes anywhere between three to five hours, and usually requires three treatments a week. Only a small amount of blood is outside of the body at one time. Therefore blood must circulate through the machine many times before it is cleaned.
Are there any complications?
- Problems associated with kidney disease itself: The kidneys act as the filtration process to remove wastes and extra fluids from the body. They also balance chemicals and hormones while performing this procedure. When kidneys stop working efficiently, a patient may have problems that might include anemia, fatigue, bone problems, joint problems, itching, and leg cramping. These may not be completely cured by dialysis and may continue to cause problems.
- Site Infections: Infections at the vascular access site are a risk that hemodialysis patients face, particularly if the site is not cared for on a regular basis. Any time the skin is compromised, even for a valid medical reason, there is an increased risk of infection. The most common infections are caused by bacteria on the patient's skin, or in the dialysis room itself. However, some patients with kidney disease do not have normal immune resistance to infections and may acquire infections from a variety of organisms that would not ordinarily affect them.
- Bleeding: Problems with bleeding can occur at the vascular access site because the skin has been compromised. This is much less common with some of the new synthetic grafts that allow for almost complete closure of the puncture holes; however, it is still a possible complication. Because the kidneys are involved in the production of important blood factors, the patient may have other bleeding problems.
- Thin and weak bones: Although this is primarily a problem associated with the underlying kidney disease, it is important for dialysis patients to be aware of because the dialysis procedure will not necessarily correct this 100 percent. A large percentage of dialysis patients develop what is called renal osteodystrophy. This results from problems with the metabolism of calcium and phosphorus and causes bones to become thin and weak or malformed. Older patients and women who have gone through menopause are at greater risk for this disease.
- Itching (pruritus): Itching skin is a common complaint among patients undergoing hemodialysis and seems to become worse during or just after treatment. The condition is made worse by toxins that current dialyzer membranes can't remove from the blood. Itching can also be related to high levels of parathyroid hormone in the blood, something that is relatively common in patients with kidney disease.